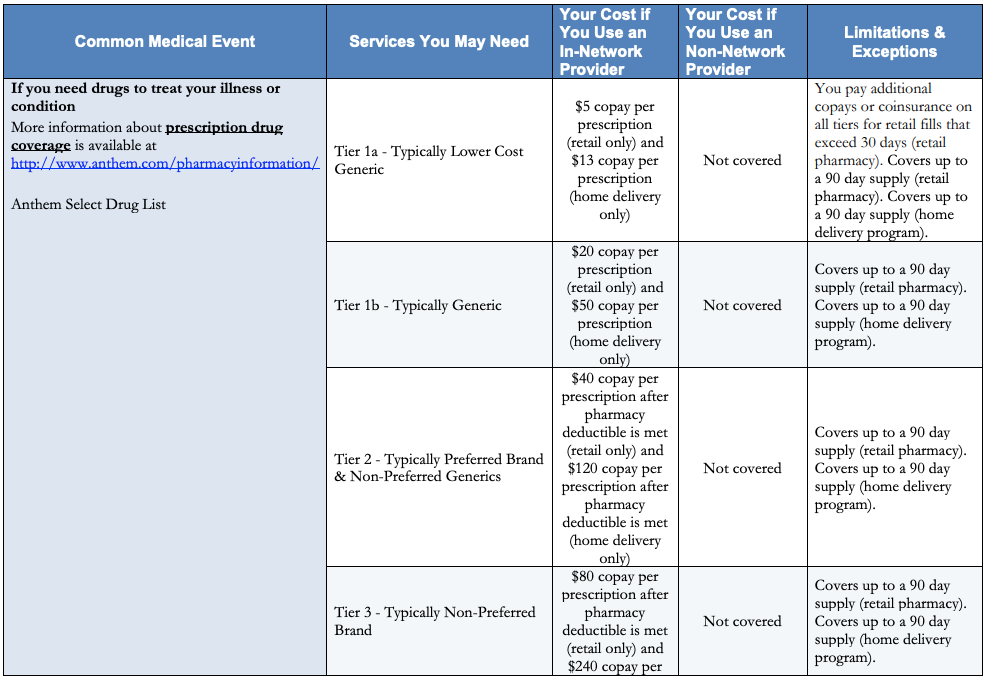
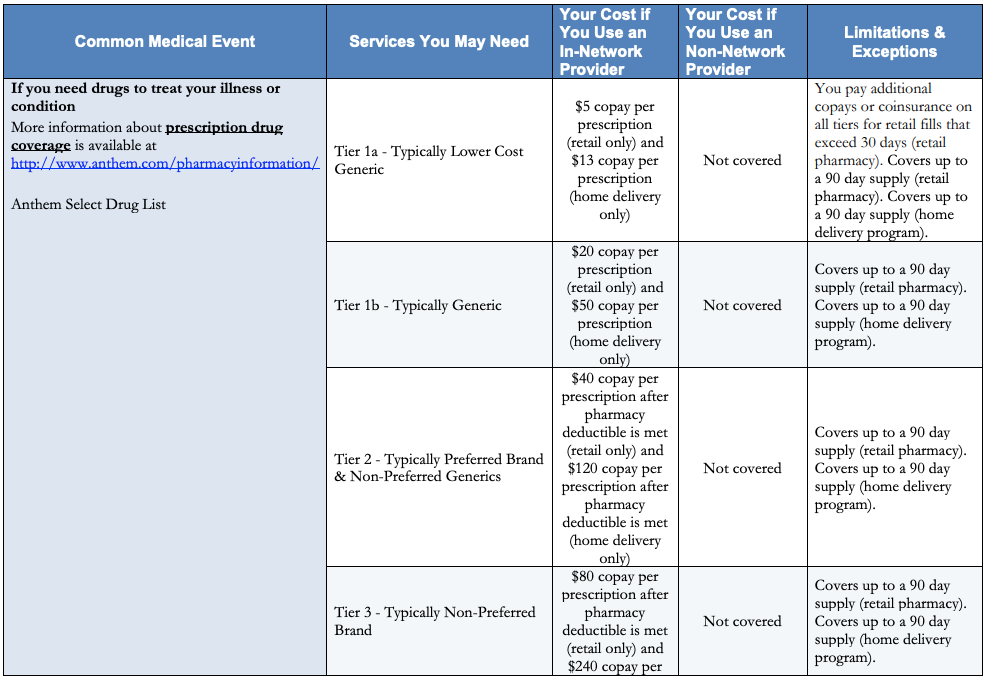
What is a Health Savings Account (HSA)? How it works: Enroll in a High Deductible Health Plan (HDHP), which means you pay for your health care before your health insurance plan begins to pay. Anthem Medicaid’s Prenatal program with. A copay is a fee that is charged for some health care services. If you receive a service that requires a copay, you pay the provider at the time of service. You can ask if there is a copay when you schedule an appointment. The list of services that will require a copay are below. This Anthem Blue Cross plan does offer additional coverage through the gap. H0544-108 Formulary or Drug Coverage. Anthem MediBlue Plus (HMO) formulary is divided into tiers or levels of coverage based on usage and according to the medication costs. Each tier will have a defined copay.
FAQs
Copays For Blue Cross Coverage


Anthem Copay Plan

Anthem Copay
Frequently Asked QuestionsQ: How do I conteact Customer Service by phone?A: For CDHP/HRA Customer Service call 866-207-8304. All other plans call 800-364-3301Q: How do I file a claim?A: If you receive emergency or authorized care from a PPO network provider, you do not need to submita claim. The network providers have agreed to to handle this process for you. If you receive services from a non-network PPO provider, you will need to submit a claim for reimbursement.You can obtain a claim from by calling Customer Service or by downloading a form on the member websiteat www.anthem.com/ca. Use a separate claim form for each patient and service provider. Occasionally, a claim is denied payment. If this happens, you and the provider of serives will receive anexplanation of denial. If you believe your claim should be paid, please call the toll-free Customer Servicenumber on you ID card. This information is also included in your EOC. Q: What is a deductible, co-insurance, and a co-pay?A: A deductible is an annual flat-dollar amount that you meet before your Anthem plan begins to pay onmedical expenses. Co-insurance is a fixed precentage cost-sharing arrangement for certain services you receive after the deductible has been met. Co-pays are flat dollar amounts that you pay for certain servicesat the time you receive care. Q: How does the out-of-pocket maximum work?A: The out-of-pocket maximum limit is the maximum dollar amount of deductible and/or coinsuranceexpense paid by a covered person and/or family for covered services (except prescription drug and mentalhealth/substance abuse charges) in a benefit period. After you reach your out-of-pocket limit, Anthem covers100 percent of the eligible charges for the remainder of the benefit period (except prescription drug andmental health/substance abuse charges). Copay may still apply depending on your Anthem plan.Q: What is Coordination of Benefits (COB)?A: COB usually applies when you or a covered dependent are covered by multiple health plans at the sametime. For example, you and your spouse have coverage through each others employers; you each coveryourself and/or dependents. The provision is designed so that the payments by all plans do not exceed 100percent of billed charges for the covered services. The provision also designates the order in which themultiple health plans are to pay benefits. Under a COB provision, one plan is determined to be primary andits benefits are applied to the claim first. The unpaid balance is usually paid by the secondary plan to the limitof its responsibility. Benefits are thus 'coordinated' among all of the health plans. Q: Why did I receive a Coordination of Benefits questionnaire and do I have to return it?A: You received a Coordination of Benefit questionnaire because we appear to have incomplete informationabout you or your covered dependents or we received information that indicates that you or your covereddependents may be covered by more than one health plan. Completing the questionnaire and returning it tous will enable us to maintain accurate information with regard to you and your dependents health carecoverage. Often, we may need to suspend the payment of your medical claim until we receive your COBquestionnaire response, so it’s important to make sure you respond.Q: What happens to my coverage if I am no longer employed by HP?A: There is a federal law known as COBRA which might apply. If COBRA applies to you, you have anopportunity to remain covered under HP's coverage for some period of time, provided you pay the fullamount of your premium. You may also be eligible to convert to an individual policy of coverage offered byAnthem. This is typically known as a 'conversion privilege'. Note: If a service was authorized by us beforetermination, but is not rendered until after your coverage ends, Anthem is not responsible for paying benefitsfor such services. Q: How do I print a temporary ID card?A: Login at www.anthem.com/ca. If you have not visited this site before, you will need to establish an accountby clicking on the “Register Now” in the Member Login box. Upon login, click the the ‘Customer Care’ box,then select the “Print Temporary ID Card” link.Q: What emergency coverage do I have while I am traveling?A: With Anthem coverage, you can be rest assured that if you need emergency or urgent care while out oftown, your benefits travel with you. Just remember to pack your Anthem ID card. If you are traveling in theUnited States, you will have the same coverage you have while at home. And since your Anthem plan givesyou access to the Blue Cross and Blue Shield provider networks across the country, you can receive in-network level benefits while on the road.Q: Where do I compare health care costs?A: Anthem’s health site includes our industry-leading transparency tool, Estimate Your Cost. A demonstrationof this tool is located under the Featured Demos section of this site or just click here. CDHP HRA Frequently Asked Questions:Q: How is my HRA funded?A: If you are enrolled in Anthem's CDHP plan, HP will fund an annual Health Reimbursement Account (HRA)on your behalf. The HRA is available to help pay your out-of-pocket expenses during the year for you andyour covered family members. If you enroll in the Anthem CDHP plan after January 1st, your HRA amountwill be prorated based on the remaining months in the calendar year. Q: What type of services may I pay for with my HRA funds?A: When you have eligible medical expenses, they'll be paid from your HRA first if funds are available.Health care services such as doctor’s office visits, lab tests and surgeries are covered. Check your BenefitBooklet for more information on covered services.Q: What is traditional health coverage?A: Similar to a PPO plan, after you meet your deductible, you pay coinsurance (a percentage of theprovider’s charges) when you visit a network provider. You’ll pay more if you visit an out-of-network provider.Check your Benefit Booklet for more information on coinsurance amounts.Q: How do I check my health account balance?A: Log on at Anthem.com/ca. You can keep track of your account and balance and get details on yourmedical claims. You may also call the Customer Service number on your ID card.Q: If I leave this CDHP/HRA plan, what happens to my HRA funds?A: You will forfeit (lose) the HRA funds if you leave the plan unless you terminate employment and continuecoverage through COBRA. Q: What services does the CDHP/HRA plan cover?A: The CDHP/HRA plan covers medical expenses, which generally include expenses covered by a typicalhealth plan. Check your Benefit Booklet to see some of the services covered by your plan.Q: What about preventive care services like mammograms and physicals?A: Anthem's CDHP plan covers preventive care services like physical exams, immunizations andmammograms at 100% in network. There’s no deduction from your HRA nor do you have to pay anything outof your own pocket when you receive care from a network provider.